Neutrophils are critical immune cells for antimicrobial defense, but they can exacerbate a number of diseases, perhaps including COVID-19. The traditional approaches to study neutrophils in animal models are limited in specificity and effectiveness. EPFL scientists have now identified the problem and have developed a new, optimized model for studying the role of neutrophils in the context of disease.
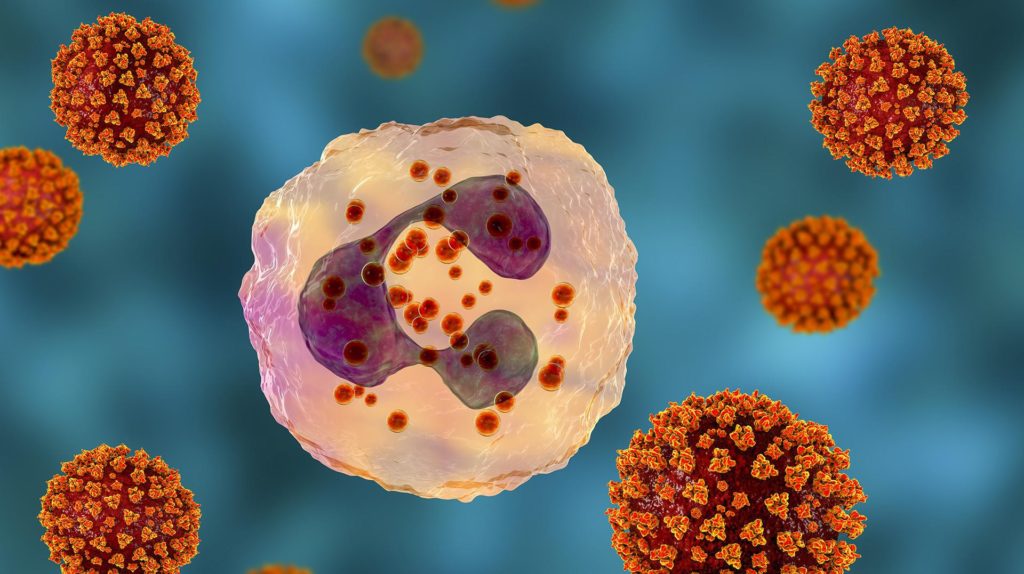
As the COVID-19 pandemic continues to spread, researchers are turning their attention to the virus’ biology, mechanism of action, and possible treatments. One of the targets are a group of immune cells called “neutrophils”, which have been reported to infiltrate the respiratory tract of patients who have died from COVID-19.
The idea is that in their attempt to attack the virus, neutrophils might be making the disease’s symptoms even worse by invading the lungs and exacerbating inflammation there. In order to find out if this is actually the case, scientists may use a mouse model whose neutrophils they deplete with “anti-neutrophil” antibodies.
The approach is used widely for studying neutrophils in a number of different conditions, including autoimmune diseases, chronic infection or inflammation, wound healing, and even some types of cancer. However, the neutrophil-depletion model is only partially effective, lacks specificity, and doesn’t last long enough.
Now, scientists led by Etienne Meylan at EPFL, have identified the source of the problem and have developed an alternative model that addresses its shortcomings. The work is published in Nature Communications.
By attempting to deplete neutrophils in mice, the animals’ bone marrow produces new neutrophils – which defeats the model’s entire purpose. The researchers have now identified these neutrophils, and determined that the reason they survive is because they have a lower chance of being targeted by the antibodies.
To address this, the scientists have developed a double antibody depletion strategy that enhances neutrophil elimination. The method increases the killing rate of the antibodies, resulting in a profound, specific and long-lasting reduction in neutrophil numbers in blood and tissues.
“Our study could be useful to address the functional importance of neutrophils in acute or chronic infection, in inflammation or in cancer,” says Meylan. “In particular, transgenic mouse models of SARS-CoV-2 infection coupled to our standardized neutrophil depletion strategies may help establish a causal link between this innate immune cell type and COVID-19.”
Other contributors
- Lausanne University Hospital (CHUV)
- Swiss Cancer Center Léman
- INSERM, France
- Massachusetts General Hospital Research Institute
- University Duisburg–Essen
Funding
- Swiss National Science Foundation
- ISREC Foundation
- Chercher et Trouver Foundation
- Nuovo Soldati Foundation
- MGH ECOR
- NIH
- Fondation pour la Recherche Médicale
- French National Cancer Institute
- Ligue contre le cancer
- LABEX DevWeCan
References
Gael Boivin, Julien Faget, Pierre-Benoit Ancey, Aspasia Gkasti, Julie Mussard, Camilla Engblom, Christina Pfirschke, Caroline Contat, Justine Pascual, Jessica Vazquez, Nathalie Bendriss-Vermare, Christophe Caux, Marie-Catherine Vozenin, Mikael J. Pittet, Matthias Gunzer, Etienne Meylan. Durable and controlled depletion of neutrophils in mice. Nature Communications 02 June 2020. DOI: 10.1038/s41467-020-16596-9
